What Does Ambulatory Referral Mean? Decoding this Key Healthcare Mechanism
What Does Ambulatory Referral Mean? Decoding this Key Healthcare Mechanism
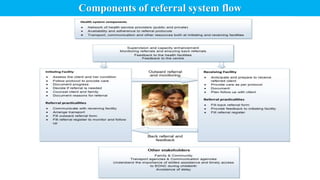
Ambulatory referral represents a fundamental yet often misunderstood element of modern medical care—one that bridges general practice with specialized services through coordinated referral pathways. At its core, an ambulatory referral is a clinical communication that transfers a patient from a primary care provider to a specialist for evaluation, diagnosis, or treatment, all within an outpatient setting. This process, supported by structured healthcare systems, ensures continuity and precision in patient management.
But what does ambulatory referral truly mean in practice? It signifies more than just a referral slip; it is a strategic, regulated exchange designed to streamline care and improve outcomes across medical specialties.
Defined by standardized protocols, ambulatory referral operates as a critical link in the healthcare continuum.
It begins when a patient’s general physician identifies a condition requiring expert intervention—such as orthopedic, cardiological, or neurological expertise—and formally directs the transfer. Unlike inpatient admissions, ambulatory referrals are timed for outpatient visits, enabling timely diagnosis without hospitalization. These referrals typically follow a clear structure: patient demographics, clinical summary, presenting symptoms, relevant medical history, and specific referral goals—not just a vague request.
“This isn’t just about sending a patient,” notes Dr. Elena Torres, a healthcare systems specialist. “It’s about delivering contextually relevant care at the right time.” Ambulatory referrals thus preserve clinical focus while preventing fragmented treatment across facilities.
Central to the operational efficiency of ambulatory referral is a well-defined workflow that respects both provider time and patient needs.
The process generally unfolds in three key stages:
- Initiation: The primary care provider, often a family physician or internist, conducts an early assessment and determines if specialty care is indicated. This initial determination is documented with clinical justification to justify the referral’s clinical necessity. “Clinicians must balance urgency with resource appropriateness,” observes Dr.
Marcus Lin, a health policy analyst. “Not every symptomatic patient requires immediate specialist input—referrals must be targeted.”
- Transmission: The referral document is securely transmitted—via electronic health records (EHR), dedicated referral systems, or digital platforms—to the designated specialist clinic. Modern systems use HL7 or FHIR standards to ensure interoperability, reducing delays and errors.
This digital exchange enables seamless access to patient data, enhancing diagnostic accuracy and safety.
- Follow-Up Integration: Once consulted, the specialist evaluates the patient and reports outcomes directly back to the primary care team. This bidirectional communication ensures continuity, allowing the primary provider to adjust treatment plans based on specialist findings. The closed loop of referral—transfer, assessment, return information—epitomizes coordinated care.
Why Ambularatory Refers Matter More Than Ever In an era marked by rising chronic disease burden and increasing healthcare complexity, ambulatory referral systems have become indispensable.
Studies indicate that well-structured referrals reduce unnecessary specialist visits by up to 40%, lowering costs and improving system capacity. For patients, this means faster access to appropriate care and reduced risk of delayed diagnosis. But challenges persist: fragmented records, inconsistent referral quality, and administrative burden continue to hinder effectiveness.
To address these, health systems are investing in interoperable platforms, decision-support tools, and standardized referral templates.
Consider orthopedic referrals: A primary care doctor identifies persistent knee pain unresponsive to conservative treatment, initiates an ambulatory referral with clear documentation of physical exam results and prior imaging. The physi desperately needs the referring physician’s input to decide on MRI relevance or surgical consultation.
Without a precise referral, the patient risks prolonged undiagnosed pain or missed critical interventions. “When referrals are clear and timely,” says Dr. Torres, “patients move through the system with purpose—not proper care or waste.”
Ambulatory referral is not merely administrative logistics—it is a clinical necessity that strengthens care quality.
Its design embeds accountability, context, and coordination into every patient journey, ensuring that specialty expertise is leveraged where it matters most. As healthcare evolves toward value-based models, the efficiency and accuracy of ambulatory referral pathways will only grow in importance. For providers, patients, and payers alike, understanding the precise meaning and impact of this mechanism is key to navigating modern medicine effectively.
In essence, ambulatory referral encapsulates a core principle of integrated care: seamless, intelligent movement between provider levels, driven by clinical need, supported by technology, and anchored in patient-centered outcomes.
As long as healthcare prioritizes accessibility, safety, and precision, the concept of ambulatory referral will remain a cornerstone of effective outpatient management.



Related Post

Buffalo Ny Zip: Revolutionizing Connectivity in America’s Rust Belt
.png)
At 34, Married and Creating Equal Lives: Unpacking Age, Marriage, Salary, and Shared Futures

Master the Essentials: Ec601 Control System & Instrumentation Deep Dive Based on Makaut Question Paper

