Tyrus Health Issues Today: Unmasking Rising Chronic Conditions in Modern Society
Tyrus Health Issues Today: Unmasking Rising Chronic Conditions in Modern Society
A growing swell of untreated and undertreated health conditions is reshaping Tyrus health landscapes, underscoring urgent challenges in personalized medicine, access to care, and public health awareness. From diabetes and cardiovascular disease to mental health disorders and metabolic syndrome, chronic illnesses now dominate the medical agenda—affecting millions across Tyrus and beyond. Recent data reveals that over 60% of adults in the region live with at least one chronic condition, many managed through fragmented care systems.
Behind these statistics lie real stories: a 42-year-old teacher struggling with uncontrolled type 2 diabetes; a middle-aged man grappling with depression linked to untreated hypertension; and young women burdened by anxiety exacerbated by pandemic-related isolation. These cases illustrate a broader crisis: rising health issues are not only straining individual lives but also testing the resilience of healthcare infrastructure.
Among the most prevalent health challenges today, cardiovascular diseases remain the leading cause of mortality and long-term disability in Tyrus, accounting for nearly 25% of all deaths annually.
High blood pressure, obesity, and diabetes fuel this epidemic, creating dangerous synergies that accelerate arterial damage and increase stroke risk. “We’re seeing earlier onset and more aggressive forms,” notes Dr. Elena Marquez, cardiologist at Tyrus Regional Medical Center.
“Patients now present with heart conditions previously confined to older populations—often linked to sedentary lifestyles, poor nutrition, and chronic stress.” Beyond physical strain, the psychological toll is profound, with many individuals isolating due to fear of hospitalization or treatment failure. The rise of electronic health monitoring and community-based prevention programs offers hope, but gaps in access and health literacy persist.
Mental health disorders have surged in visibility—and urgency—across Tyrus public health discourse.
Anxiety, burnout, depression, and post-traumatic stress now affect nearly one in three residents, a stark contrast to pre-pandemic prevalence rates. “Society has finally acknowledged what was long ignored: mental well-being is inseparable from physical health,” observes Dr. James Tran, a psychiatrist specializing in workplace and trauma-related care.
“Yet stigma, workforce shortages in mental health services, and inequitable access delay intervention for most.” Schools, workplaces, and primary care clinics are increasingly integrating behavioral assessments, but demand far outpaces supply. Young professionals report heightened stress from economic uncertainty and digital overload, while older adults face loneliness and delayed diagnosis. This mental health wave demands systemic reform, from policy-level funding to culturally competent support networks.
Diabetes continues to emerge as a television health issue of Tyrus’ time—impacting over 400,000 residents with type 2 diabetes and forcing sustained management that shapes daily routines. Excess weight, poor diet, and genetic predisposition fuel the rise, yet early detection remains elusive. Many live with undiagnosed or suboptimal control, increasing risks of kidney failure, blindness, and nerve damage.
“So many individuals are managing without regular check-ups or medication_access,” explains Dr. Fatima Al-Jawi, a leading endocrinologist. “Telehealth has helped, but not everyone can navigate digital tools or afford continuous care.” Success stories—like Tyrus Diabetes Alliance’s community screenings—show impact: early diagnosis, education, and peer support reduce complications by up to 30%.
Yet broad-scale prevention through policy and public health campaigns remains underinvested.
Underlying these chronically rising health burdens are socio-economic and environmental determinants. Low-income neighborhoods face compounding disadvantages: limited green space for physical activity, higher exposure to pollution, and reduced access to nutritious foods.
Racially and ethnically diverse communities report disproportionately higher rates of hypertension, liver disease, and anxiety—reflecting generations of systemic inequity. “Health is not just a personal responsibility; it’s a societal duty,” states Dr. Marquez.
“We need targeted outreach, culturally aware care, and affordable preventive services to close these gaps.” The integration of social services with clinical care is emerging as a model, linking food assistance, housing support, and mental health resources directly into healthcare networks.
Technological advances offer promising tools but also raise ethical considerations. Wearable monitors, AI-driven diagnostics, and mobile health apps enhance early detection and patient engagement—yet data privacy and equitable access remain critical.
“Technology should empower, not exclude,” cautions Dr. Tran. “If only some populations benefit, we deepen disparities rather than solve them.” Currently, only 55% of eligible Tyrus residents use such tools, often due to cost, literacy, or distrust in digital systems.
Hybrid care models—blending high-tech innovation with human-centered support—are proving most effective, particularly when paired with community health workers who bridge trust and literacy barriers.
Looking ahead, the path forward demands coordinated action across policy, education, and clinical innovation. Expanding community health hubs equipped for screening, counseling, and chronic disease management could reduce hospital burdens and improve outcomes.
Policy initiatives focused on sugar taxes, urban planning for active living, and mental health parity laws are already gaining momentum. Yet success hinges on public engagement and reducing systemic friction. Every individual, provider, and policymaker holds a role—whether advocating for change, choosing preventive care, or destigmatizing illness.
As Tyrus navigates its health landscape, the imperative is clear: robust, inclusive, and forward-thinking health systems are not luxuries but lifelines. Only through such commitment can the region break free from the grip of escalating chronic illness.
In the evolving story of Tyrus health, the numbers are stark—but so is the potential for transformation.
By addressing root causes, expanding access, and embracing innovation with equity at its core, this region can shift from crisis to resilience. The path is complex, but the blueprint exists—now lies the will to implement it.




Related Post

Unlocking Language in Math: How CurvedESymbolInMath Transforms Symbolic Representation

Helldivers 2 on PS4: A Clausy Deep Dive into Tactical Hell and PlayStation Joy
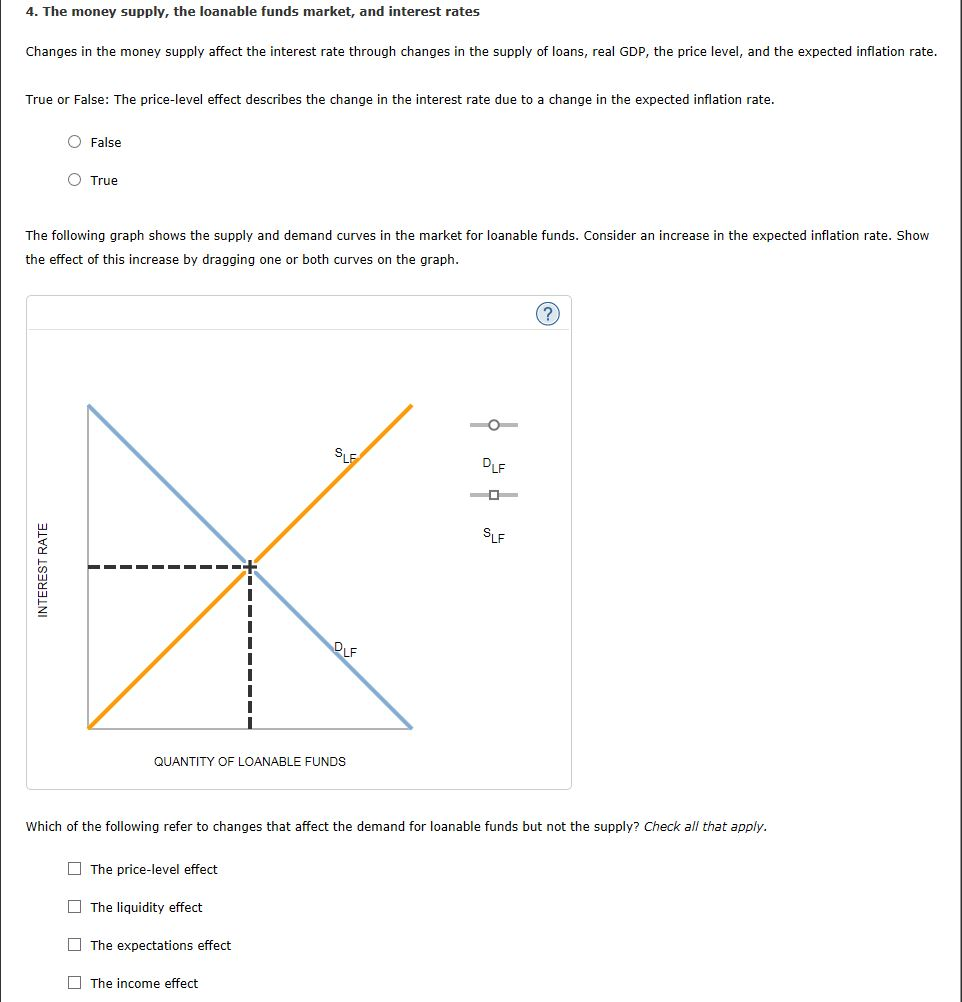
Market of Loanable Funds Unveiled: How Supply, Demand, and Interest Rates Shape Economic Growth

Alec Wildenstein Jr.: Architect of Modern Financial Journalism

