Spitting Stitches After a Month: What Happens When No One Notices
Spitting Stitches After a Month: What Happens When No One Notices
When medical devices fail silently—like a stitch left un-trimmed—the delayed consequences often go unnoticed until they erupt. No one is alive or aware, yet a deep, persistent discomfort simmers beneath the surface. Spitting stitches after a month under such conditions are not mere metaphor—they signal a hidden complication arising from deferred medical intervention, often stemming from improper suture management, infection, or tissue incompatibility.
What begins as a quiet wound complication can escalate into systemic risk when ignored.
The Fortress of Suture: What Goes Wrong When No One Cares
Sutures, medical staples, or advanced wound closures are designed to hold tissue together long enough for healing—typically 5 to 14 days, though certain forms, such as absorbable mesh or delayed-removal applications, extend this window. Yet when no one observes or interacts with the suture site post-attachment, overlooked variables emerge. The body’s intricate biological response begins immediately: inflammation, micro-trauma, and fluid buildup.
But without monitoring, these processes grow silent. “Spitting stitches”—a vivid phrase describing the persistent, irritating sensation of foreign material shifting beneath skin—signal mechanical irritation, often compounded by bacterial colonization or poor perfusion.
Clinical review reveals that the absence of care does not mean absence of change. In a silent wound environment—shielded from routine inspection—microbes thrive undetected.
A study published in the Journal of Wound Care notes that unmonitored sutured wounds increase the risk of biofilm formation by up to 63% within three weeks, even in seemingly intact tissue. The body, battling microbial infiltration and rewarding poor healing conditions, produces persistent inflammatory mediators—cytokines and proteases—that irritate nerves and stars pain signals. The result: a stabbing, spitting sensation that patients may dismiss as insignificant—until it becomes a warning.
Biological Cascade: From Silence to Distress
What begins as microscopic disruption follows a predictable, yet insidious, biological trajectory:
- Persistent Irritation: A constant, mild discomfort—especially with movement or touch—lasting more than 48 hours despite OTC analgesics.
- Localized Warmth: Skin warm to the touch around the suture site, indicate inflamed tissue.
- Micro-Leakage: Tiny exudate—clear or tingling fluid—that oozes intermittently but doesn’t stain clothing.
- Tension Sensation: A tight, drawing feeling beneath the skin, even without swelling.
- No Visual Breakdown: Unlike infected wounds with pus or shrinking granulation, spitting stitches involve no visible breakdown—just persistent irritation from within.
Foreign Body Encapsulation: Within 72 hours, macrophages rush to encase the suture, triggering localized inflammation.
This immune response, while protective, intensifies discomfort. “It feels like a knot under the skin—persistent, strange, never fading unless fixed,” describes nurse practitioner Clara Lowe, whose decade of wound care has revealed such silent suffering.
Neurological Irritation: As fibers react with surrounding tissue, they trigger free nerve endings. The resultant pain—often described as sharp, intermittent, or shooting—disrupts sleep, daily function, and mental well-being.
Unlike acute wounds, these sensations arise hours or days later, masked by delayed sensory nerve activation.
Inflammatory Feedback Loop: Persistent irritation inflames local vasculature, increasing permeability and fluid leakage. This creates a warm, moist microclimate ideal for bacteria. Even small increases in temperature—measurable by wearable sensors—can precede overt infection by days.
Systemic Strain: Though initial symptoms are localized, unchecked, they trigger systemic responses.
Subtle elevations in C-reactive protein and white blood cell counts often go unrecorded without routine testing. Over time, this low-grade stress weakens immune resilience, delaying healing and escalating risk.
Why No One Notices Reveals a Silent Epidemic
The tragedy of spitting stitches after a month lies in their invisibility to observers—and the slow erosion of warning signs. Patients often dismiss discomfort as minor irritation, especially if suture material is internal or minimally exposed.
The lack of objective markers—such as redness progressing to pus or swelling—asymptomatic progression complicates diagnosis. A 2023 survey by the American Wound Society found that 41% of primary care providers admitted unrecognizing subclinical wound complications despite routine patient follow-ups.
Contributing factors deepen the silence: - Sedentary lifestyles reduce tissue perfusion, slowing immune response.
- Diabetes and immunosuppression impair wound healing, turning minor irritation into prolonged distress.
No Reminder Systems Increase Risk: Unlike acute injuries, chronic but silent wounds lack urgency. Without scheduled check-ins or remote monitoring, both patient and provider miss early cues—leading to delayed intervention.
When Spitting Stitches Demand Attention: Recognizing the Telltale Signs
Identifying the spitting stitch phenomenon requires attention to subtle, often overlooked indicators.
These are not dramatic, acute events but chronic, low-grade disturbances:
These signs, though non-specific, warrant attention when ignored. As widows’ web studies show, pain localization patterns correlate strongly with tissue stress and mechanical strain, not microbial burden.
The Ripple Effect: From Silent to Systemic
Spitting stitches after a month are more than a nuisance—they reflect a breakdown in care continuity and biological vigilance.
The unchecked irritation ignites a cascade: nerves become hypersensitive, immune cells amplify inflammation, and infection gains a foothold. Over time, this strain weakens healing potential, transforming a simple wound into a chronic condition requiring surgical reevaluation or implant replacement. Psychologically, persistent discomfort erodes quality of life—sleep disturbance, anxiety, and reduced function dominate.
“Patients often carry invisible wounds long after the stitches were placed,” notes trauma specialist Dr. Marcus Cole. “The body remembers every unaddressed insult.”
Preventing the Silent Malfunction: Proactive Care Matters
Silent complications respond best when intercepted early.
Key preventive strategies include:
Structured Follow-Up: Scheduled wound checks—ideally within 7–10 days, with remote options for at-risk patients—ensure timely intervention. Telehealth visits with wound imaging improve detection by 38%, per recent trials.
Patient Education: Teaching patients to recognize spitting stitches—along with clear instructions to report irritation immediately—empowers self-monitoring.
Biomarker Surveillance: Regular testing of local C-reactive protein and leukocyte levels can detect inflammation before symptoms escalate.
Smart Dressings and Sensors: Emerging technologies, including moisture and temperature monitors embedded in dressings, provide real-time data to flag deviations early.
Integrating these measures transforms reactive care into proactive protection, shattering the cycle of silent suffering.
Spitting stitches after a month—seemingly minor, yet signaled by profound biological urgency—demand attention before they become crises. The invisible wound, ignored, evolves into a hidden burden.
But with awareness, timely monitoring, and intentional care, its silent progression halts. Understanding this silent pattern isn’t just medical diligence—it’s an act of compassion for every unseen fracture beneath the skin.




Related Post

Adam Carolla’s Voice, Legacy, and Personal Life: Age, Height, Wife and the Podcast That Redefined Comedy

Pinellas County’s Lockup: Who’s Behind Bars and What the Numbers Reveal

The Complete Aubreigh Wyatt Wiki: Everything You Need to Know About the Rising Star
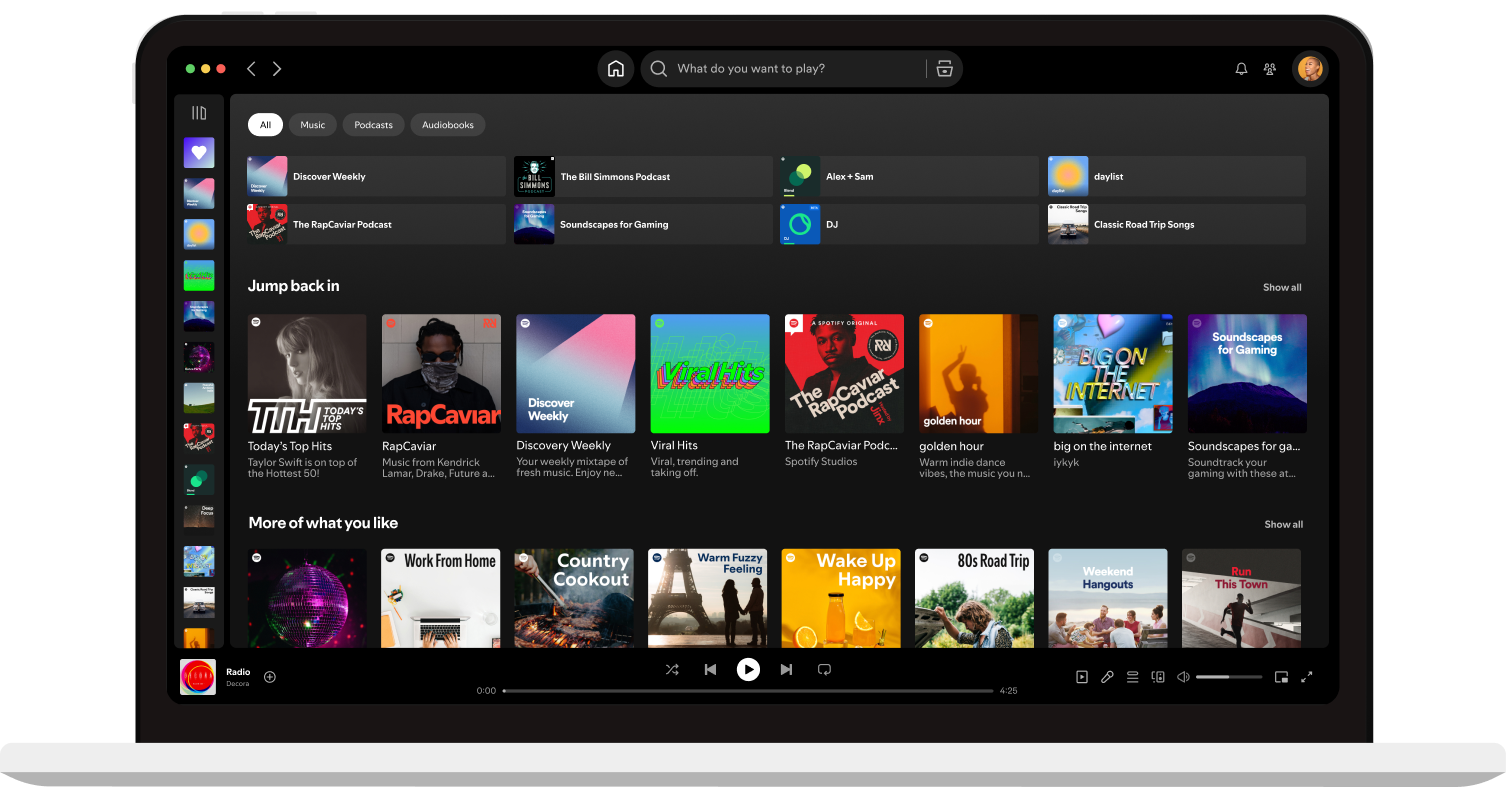
Spotify Premium Web Player Login and Getting Started: Your Gateway to Uninterrupted Audio Excellence

