HIV/AIDS in Indonesia: Projected Trends and Challenges by 2025
HIV/AIDS in Indonesia: Projected Trends and Challenges by 2025
Indonesia faces a critical juncture in its long-standing battle against HIV/AIDS, with 2025 poised to mark a pivotal moment defined by both encouraging progress and persistent challenges. Despite sustained public health interventions, shifting social dynamics, and evolving epidemiological patterns, projections indicate that the country must accelerate efforts to meet its 2025 targets. With approximately 100,000 people living with HIV, tuberculosis linked to HIV, and new infections remaining at a worrying level—particularly among key populations—Indonesia’s health authorities and international partners are confronting a complex landscape.
As data reveals changing demographics among those affected, understanding current trajectories and emerging barriers is essential to preventing setbacks and advancing toward epidemic control.
The latest statistics paint a nuanced picture: as of mid-2024, Indonesia reported over 100,000 people living with HIV, with transmission concentrated among men who have sex with men (MSM), people who inject drugs (PWID), sex workers, and transgender individuals. New infections rose slightly in recent years, clocking in at approximately 8,500 new cases annually among adults, according to UNAIDS and Indonesia’s Ministry of Health.
This uptick, though modest, underscores vulnerabilities within marginalized communities where structural barriers—stigma, criminalization risks, and limited access to testing—hinder effective prevention and treatment. “Even with expanded services, marginalized groups often avoid health systems due to fear of discrimination,” notes Dr. Siti Nurhaliza, an epidemiologist at Gadjah Mada University.
“This hidden population remains the wildcard in our projections.”
Key Projections for 2025: The Path Remains Tight By 2025, modeled forecasts project a plateau—possibly a slight decline—if current interventions continue unchanged. With sustained activist efforts, funding levels stabilizing, and incremental progress in ART (antiretroviral therapy) coverage, the national target of treating 95% of people living with HIV remains within reach. Currently, roughly 85% receive life-saving treatment, a significant improvement from just 50% a decade ago, per Indonesia’s National AIDS Program (UNAIDS Indonesia, 2024).
However, treatment access is uneven: rural areas and eastern provinces lag behind Java and Bali by 15–20 percentage points. Moreover, early diagnosis remains a challenge—only about 40% of new cases are identified annually, meaning nearly 60% live undiagnosed, increasing transmission risks and delaying care. Across the region, the convergence of aging HIV-positive populations and persistent youth transmission creates a dual responsibility for health planners to maintain momentum while adapting strategies.
Several structural and societal challenges threaten to derail progress.
Foremost among them is persistent stigma, deeply rooted in cultural norms and legal ambiguities. Although Indonesia decriminalized same-sex conduct in 2008, local implementations remain inconsistent, and criminal penalties loom for some groups, sharply limiting outreach and trust. “Stigma isn’t just a social issue—it’s a public health barrier,” states Dr.
Arief Wibowo, head of service delivery at the Jakarta-based AIDS Support Organization (YGTH). “Fear of exposure stops people from seeking testing, treatment, or support.” In parallel, budget constraints and uneven health system capacity impede program scalability. While the government increased devoted HIV/AIDS funding by 12% from 2023, resource gaps persist in community testing, cultural competency training, and psychosocial support.
These constraints are magnified in remote islands like Papua and Maluku, where outreach infrastructure is limited and health workers are scarce.
Emerging epidemiological trends further complicate projections. Rising syphilis and hepatitis C co-infections—largely through unprotected sex and shared drug equipment—exacerbate AIDS-related morbidity and mortality, placing additional strain on healthcare workers and facilities already stretched thin. Meanwhile, new infection routes linked to urbanization and digital connectivity—such as transactional sex amplified by online platforms—introduce novel transmission dynamics less addressed by existing prevention programs.
“Our prevention tools were built for the 2000s,” observes Dr. Nurhaliza. “Digital ecosystems are outpacing our adaptive public health responses.” To counter this, targeted campaigns leveraging mobile technology, peer educators, and inclusive messaging in multiple languages are being rolled out, but scaling these effectively requires sustained political will and funding.
Significant opportunities exist to strengthen Indonesia’s 2025 strategy.
Strong political commitment—evident in President Jokowi’s repeated public acknowledgments of HIV as a national priority—has elevated visibility and mobilized resources. Community-led organizations and networks continue to fill critical service gaps, particularly in testing, counseling, and linkage to care, often reaching populations symbolic health systems ignore. Anticipated advances in biomedical prevention, including long-acting injectable pre-exposure prophylaxis (PrEP) and pre-exposure vaccine trials, offer transformative potential.
“If Indonesia integrates PrEP into its national HIV strategy by 2025, we could sharply reduce new infections among MSM and PWID,” says Dr. Siti Nurhaliza. Equally vital is stronger data systems to track transmission patterns, especially among youth and migrant populations straddling urban and remote regions.
With improved surveillance, targeted interventions can become more precise and efficient.
International partnerships and funding remain indispensable. Organizations including UNAIDS, PEPFAR, and the Global Fund provide critical technical support and financing, enabling scale-up of testing, treatment, and prevention. Yet shifting global health priorities and donor fatigue pose silent threats: sustained pledges are necessary to maintain gains as new global health challenges emerge.
Altru Karayaan, Indonesia’s HIV Program Head at UNAIDS, cautions: “2025 is the year we either lock in momentum or lose hard-won progress. Without bold, inclusive action, Indonesia may not meet its epidemic control vision.”
While Indonesia’s trajectory toward an AIDS-free future remains within reach, the path forward demands relentless attention. The data underscores that progress hinges not only on medical tools but on social transformation—eliminating stigma, expanding access, and centering the voices of those most affected.
With strategic investment, adaptive programming, and unwavering political resolve, the



Related Post

How to Unlock Rohan Jabeel’s Novel: Your Essential PDF Download Guide

Protect Prokaryotes From Being Broken Down — Preserving the Microbial Backbone of Life
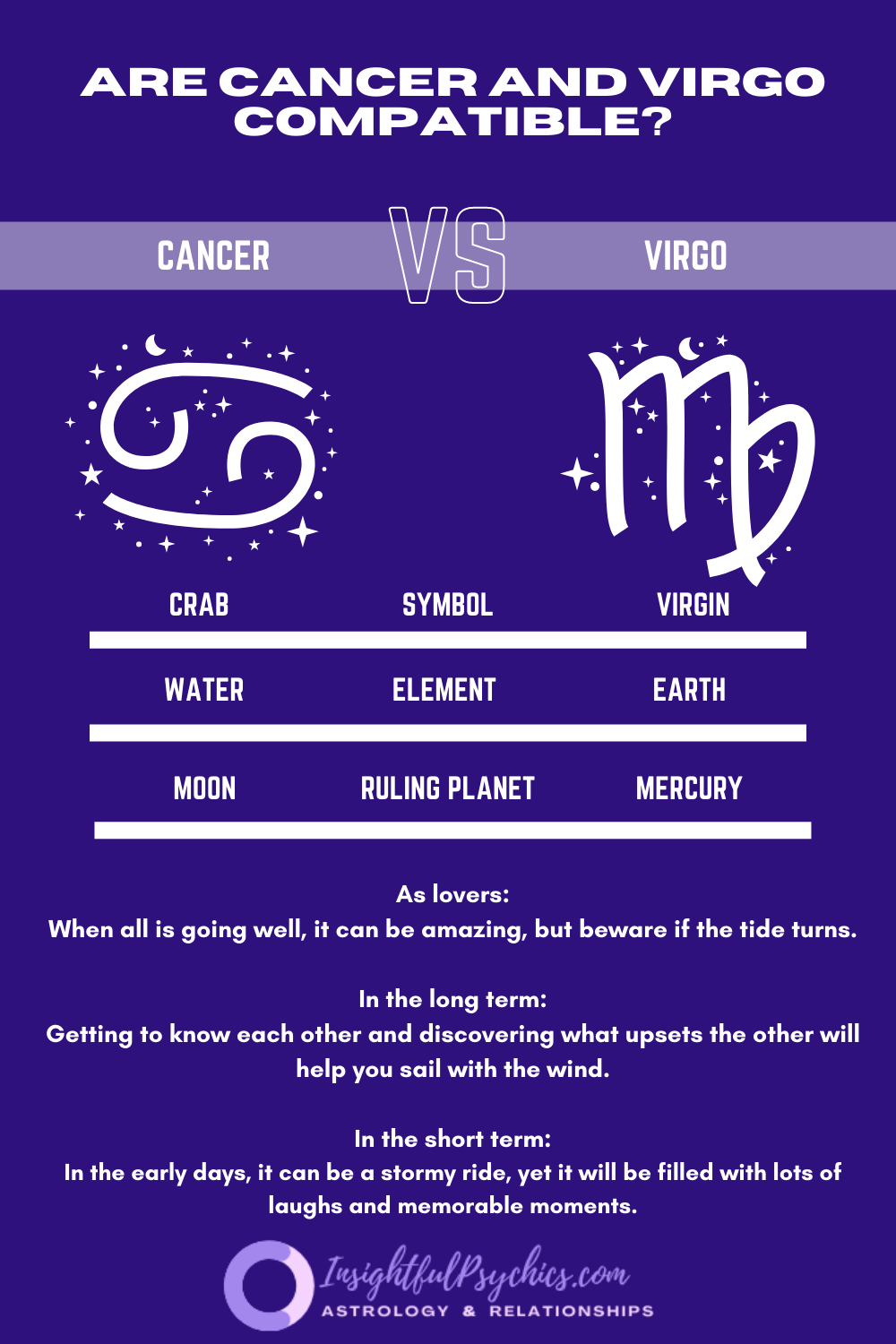
Virgo And Cancer Compatibility: A Celestial Bond Unlocking the Secrets of Love

No Mercy Mexico: Unraveling the Controversy Behind a Shocking Wrestling Phenomenon

