Hepatitis B Serology: Your Definitive Guide to Understanding the Disease Through Blood Tests
Hepatitis B Serology: Your Definitive Guide to Understanding the Disease Through Blood Tests
Flu frightening liver inflammation it’s hepatitis B, a global health challenge affecting millions—but with the right serological markers, diagnosis and management become precise and actionable. Hepatitis B Serology offers a clear window into infection status, immune response, and disease progression, transforming complex biological data into critical clinical insight. This guide distills the essentials of hepatitis B serology, empowering patients, clinicians, and public health professionals with a practical understanding of how blood tests shape hepatitis B care.
At the heart of hepatitis B assessment lies serology—the scientific analysis of antibodies and antigens in the bloodstream. These biological markers reveal whether someone is acutely infected, chronically infected, vaccinated, or immune. The World Health Organization estimates over 250 million people live with chronic hepatitis B, underscoring the vital role accurate serological diagnosis plays in preventing liver damage, cirrhosis, and cancer.
Understanding the principal tests—HBsAg, anti-HBs, anti-HBc, and others—is key to interpreting test results and guiding treatment decisions.
The Core Tests: Decoding Hepatitis B Serology
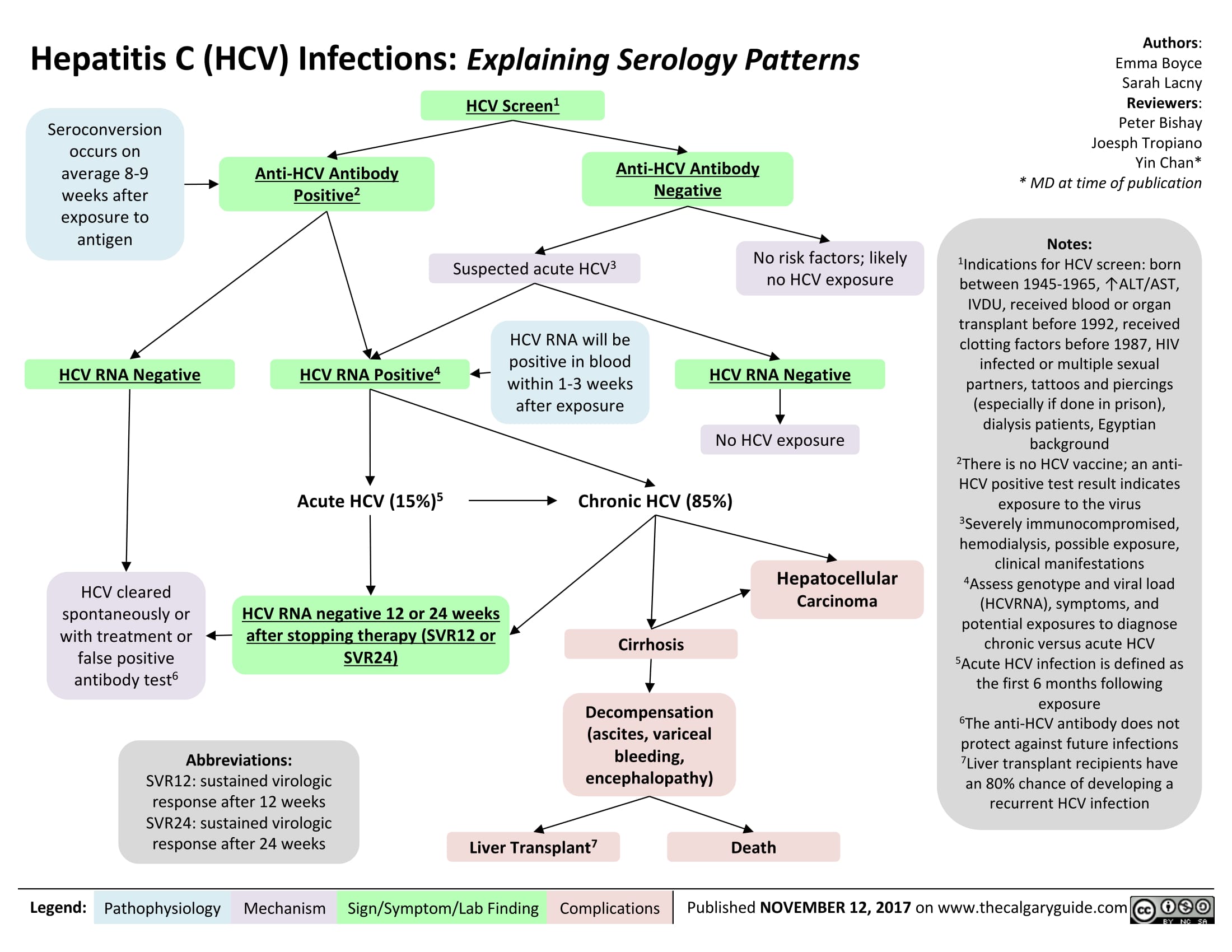
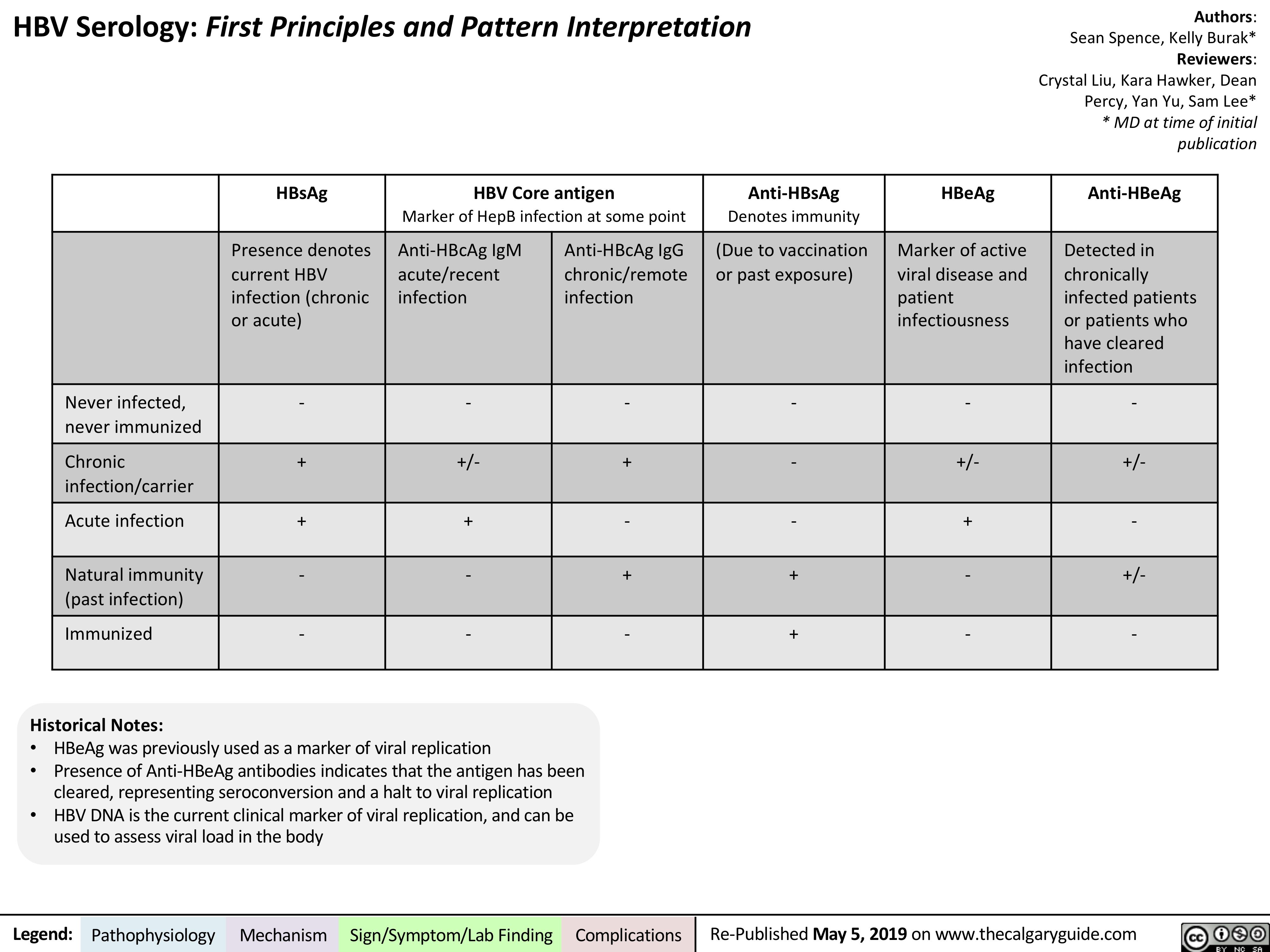
Hepatitis B serology relies on four primary markers, each offering distinct clinical intelligence: - **HBsAg (Hepatitis B Surface Antigen):** The first definitive sign of hepatitis B virus (HBV) infection. Its presence indicates active viral replication and infection—acute or chronic. Detecting HBsAg typically follows initial exposure, peaking during active replication and potentially lasting six months or more in chronic cases.- **anti-HBs (Antibody to HBsAg):** Presence of this antibody signals recovery from acute infection or successful immunization via hepatitis B vaccine. Individuals with sustained anti-HBs are largely protected and do not pose infectious risk, though immunity may wane over decades. - **HBeAg (Hepatitis B e Antigen):** A marker of high viral replication and transmissibility.
Its detection suggests active, infectious disease, particularly relevant in guiding antiviral therapy and assessing risk during pregnancy or transfusions. - **anti-HBc (Antibody to Hepatitis B Core Antigen):** Anti-HBc IgM appears early, confirming recent infection. Anti-HBc IgG remains for life after infection, serving as a serological "fingerprint" of prior exposure.
This distinction between acute and chronic infection is pivotal in diagnosis.
Additional markers include HBeAg and anti-HBe (indicating modulation of viral activity), as well as IgG subtypes of anti-HBs, which refine immune status assessments in transfused individuals or post-vaccination monitoring. Each test, when interpreted together, forms a narrative of the liver virus’s behavior in the body.
Interpreting Test Results: From Positive to Chronic Diagnosis
Clinical interpretation requires careful analysis, particularly distinguishing acute from chronic infection.A key benchmark is the persistence of HBsAg—two consecutive positive tests at 6 months confirm chronic hepatitis B. Conversely, transient HBsAg with positive anti-HBc and negative HBeAg often reflects a self-limiting acute episode. For vaccinated individuals, high titers of anti-HBs confirm immune protection, while reactors—those failing to respond—may need supplemental dose or reviewed immunity status.
Meanwhile, anti-HBc positivity universally signals HBV exposure but does not confirm active infection; only with HBsAg can chronicity be confirmed.
Examples of clinical scenarios reinforce practical understanding: - A newly symptomatic adult testing HBsAg positive with positive HBeAg suggests high viral burden and active replication—urgent antiviral intervention is warranted. - A child born to a hepatitis B mother tests positive for HBsAg but anti-HBs two months later: antibody persistence confirms chronic infection requiring long-term monitoring.
- A college student with anti-HBs and negative HBsAg after vaccination confirms successful immunization, reducing public transmission risk.
When and Why Serology Testing Matters
Testing is indicated in multiple high-stakes contexts: prenatal screening to prevent mother-to-child transmission, diagnosis following unexplained liver enzyme elevations, assessment before hepatology referrals or cancer surveillance, and post-vaccination immunity checks. In clinical practice, serology serves as a compass—guiding antiviral therapy initiation, treatment duration, and discontinuation, as well as eligibility for liver imaging and biopsies.In resource-limited settings, access to reliable serological testing remains a bottleneck.
Point-of-care testing and microarray technologies are expanding testing reach, but challenges persist in reliability, affordability, and timely result interpretation. For public health, routine serosurveys track HBV prevalence, guiding vaccination campaigns and prevention policies.
The Future of Hepatitis B Serology
Advances in molecular diagnostics and multiplex assays are refining serological precision. Emerging biomarkers, including quantitative HBV DNA alongside traditional serology, promise earlier detection of viral rebound and treatment response.Personalized monitoring—tailoring follow-up based on HBsAg kinetics and antibody durability—could soon shift hepatitis B care from reactive to proactive.
Despite technological progress, the core of hepatitis B serology remains rooted in scientifically validated markers interpreted by skilled clinicians. The clarity provided by a blood test can mean the difference between irreversible liver damage and a stability marked by sustained anti-HBs.
As global elimination targets advance, understanding serology is no longer niche—it’s foundational.
In Practice: Making Serology Accessible and Effective
Healthcare providers must balance scientific rigor with patient-centered communication. Explaining serological results in plain language helps demystify infection status, reduces anxiety, and empowers informed decisions. Integrating serology screening into routine care for at-risk populations, such as immigrants from endemic regions or high-prevalence urban clinics, is essential for early detection.Moreover, continued education for both clinicians and the public bridges knowledge gaps—ensuring serology is not just a diagnostic tool, but a cornerstone of hepatitis B prevention and care ecosystems. When combined with vaccination, harm reduction, and sustained surveillance, hepatitis B serology becomes a powerful lever in controlling a virus that still exacts heavy global tolls.
In sum, Hepatitis B Serology: A Simple Guide reveals that behind each antigen and antibody lies a story of infection, immunity, and intervention. By mastering its key markers and interpreting them with precision, healthcare teams can turn diagnostic test results into life-saving action—one test at a time.
Related Post

Warren Sapp Net Worth 2024: From NFL Stardom to Colorado Coaching Triumph – A Legacy Built on Discipline and Family

Honoring Legacy: Unearthing Lives Remembered in Concord Monitor Obituaries

Revolutionizing Legal Research: How Litematica Is Transforming Access to Justice

France vs Poland: In a Thrilling Clash, Atomic Finish and Defensive Firepower Define the Goal Highlights
.png)
