Decoding Stroke Severity with Nih Stroke Scale Group A: Why the Right Answers Save Lives
Decoding Stroke Severity with Nih Stroke Scale Group A: Why the Right Answers Save Lives
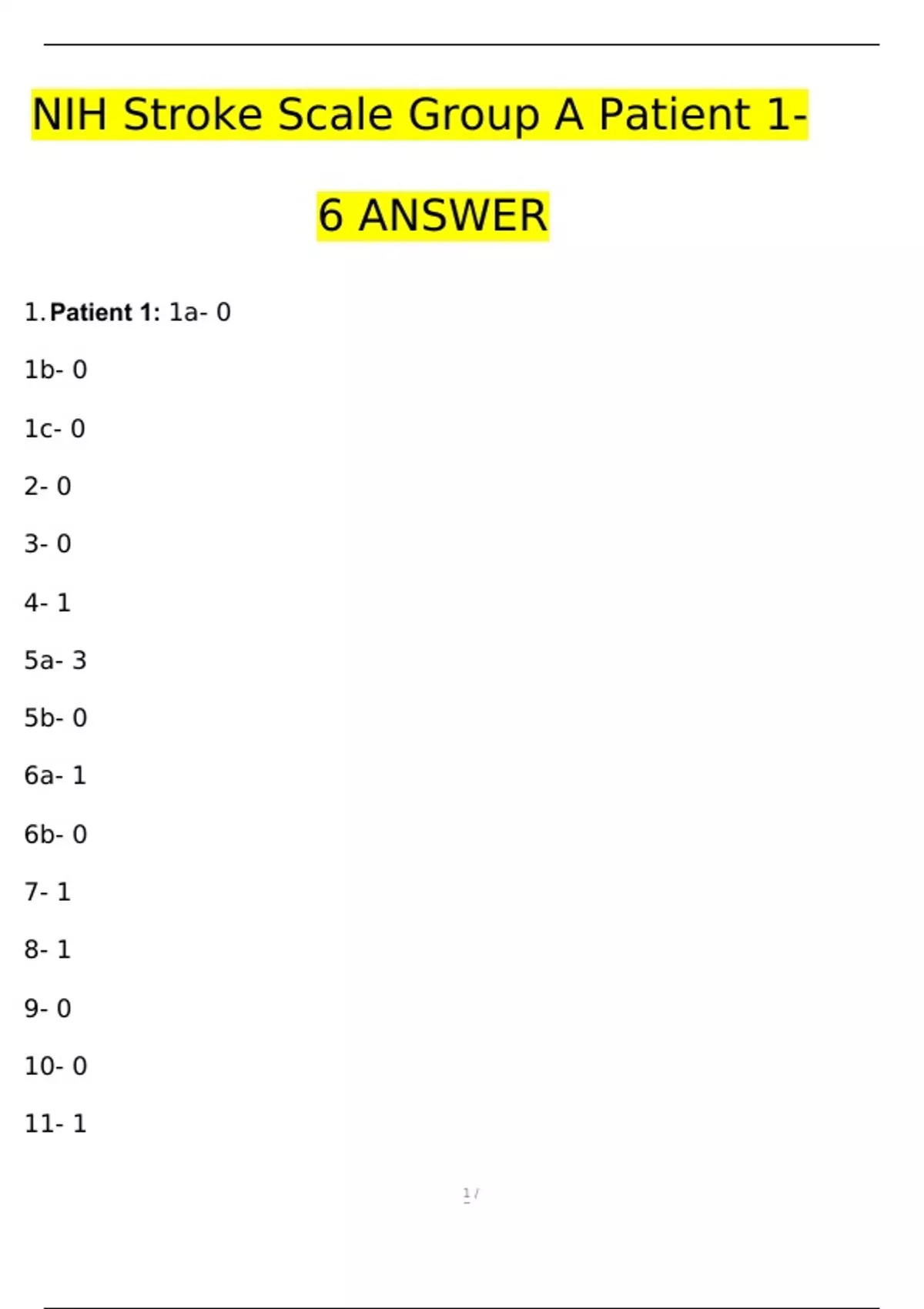
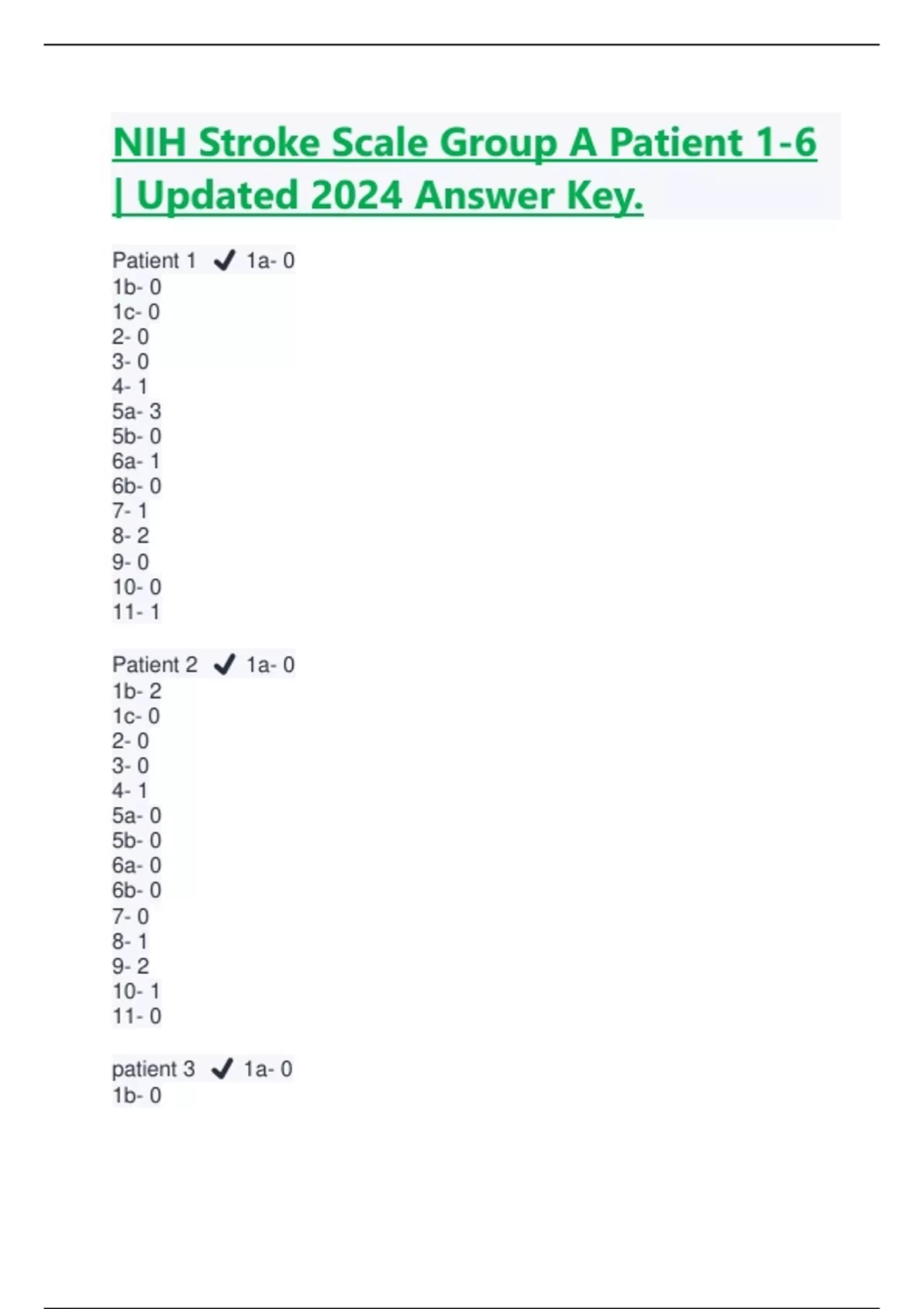
The Nih Stroke Scale Group A stands as a vital tool in the rapid assessment of acute ischemic stroke, guiding clinicians through critical early decision-making with precision and speed. Designed to evaluate five key neurological domains—level of consciousness, visual fields, motor function, facial symmetry, and verbal abilities—each question in this 15-point scale yields a score that flags stroke severity, directs treatment urgency, and informs prognosis. Correct interpretation of Group A answers enables faster thrombolysis, improves patient outcomes, and reduces long-term disability.
Each element of the Nih Stroke Scale Group A delivers decisive insights: from detecting loss of awareness to identifying cranial nerve deficits and speech impairment. “The scale is not just a digital checklist—it’s a clinical compass,” says Dr. Aiko Tanaka, a neurology specialist at Tokyo Medical Center.
“Every correct score above baseline moves us closer to time-critical interventions.”
Breakdown of Nih Stroke Scale Group A Domains:
Assessing Group A requires precision: - **Level of consciousness**: Measures alertness using scale elements like orientation and response; even minor changes signal critical brain involvement. - **Visual fields**: Detection of neglect or hemianopia reveals hidden damage requiring immediate attention. - **Motor function**: Strength testing of facial and limb muscles identifies focal weakness—key markers of ischemic burden.
- **Facial symmetry**: Asymmetry in facial movement alerts to middle cerebral artery territory involvement. - **Verbal abilities**: Speech fluency, repetition, and word comprehension test linguistic pathways often compromised early.
Each item is scored objectively, with no room for subjectivity.
A perfect Group A score remains around 0–5, but scores above 7 typically indicate moderate-to-severe stroke, warranting advanced imaging and treatment. “Delayed recognition of abnormal answers can mean lost brain tissue—and lost time,” states Dr. Tanaka.
“Speed and accuracy in scoring directly correlate with recovery potential.”
For instance, a patient displaying drooping of one eyelid (motor), inability to repeat a simple phrase (verbal), and right-sided facial numbness (visual/scalar testing) would score low. Conversely, near-normal responses across all domains suggest minimal injury. These answers transform raw observations into actionable clinical data.
The scale’s structured approach ensures consistency across emergency departments, stroke units, and telemedicine consultations. Standardizing evaluation improves inter-rater reliability, a known challenge in acute stroke care where seconds count. “In chaotic ERs, having a clear, scored protocol prevents cognitive overload,” explains Dr.
Yuki Suzuki, a neurocritical care researcher. “The scale’s brevity doesn’t sacrifice depth—it focuses analysts on what matters most.”
Clinical algorithms now routinely integrate Nih Stroke Scale Group A responses with CT imaging and thrombolysis windows. A patient scoring high on motor and verbal deficits, for example, is a prime candidate for intravenous alteplase—provided such therapy is administered within the 4.5-hour window.
Irreversible damage accumulates rapidly; each delayed call to stroke teams erodes recovery prospects. Beyond the emergency room, follow-up assessments using Group A tools help monitor recovery, detect complications, and guide rehabilitation. “The scale evolves from initial diagnosis into long-term recovery tracking,” notes Dr.
Suzuki. “Consistent scoring during rehabilitation allows clinicians to adjust therapy based on measurable progress or setbacks.”
Real-world data underscores the scale’s impact: stroke centers using Nih Stroke Scale Group A report consistently shorter door-to-needle times and improved functional outcomes. “When every second counts, standardized tools become lifelines,” concludes Dr.
Tanaka. “The right answer, delivered correctly, is not just data—it’s a pathway to patient survival.”
In essence, mastery of Nih Stroke Scale Group A answers is not only a technical skill but a clinical imperative. With its strong predictive validity and broad usability, this systematic approach empowers healthcare providers to act decisively, turning uncertainty into action and, ultimately, saving lives one scored item at a time.


Related Post
Who Made the Gift That Only One Company Could Invent: The Birth of the Google

MRT Workbook Step 4: Transform Your Life by Mastering the My Life Assessment
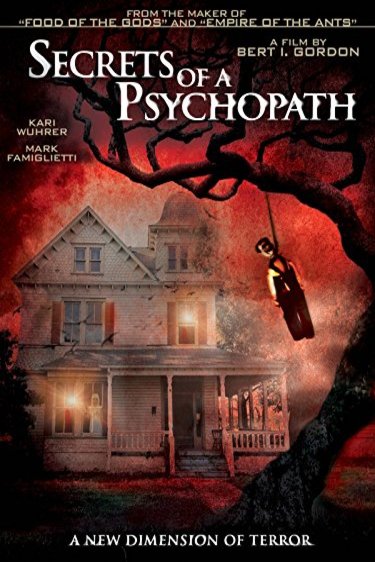
Psychopath American: The Dark Mirror of a Nation’s Soul

Astonishing Wealth: Elton Brand’s Net Worth Revealed