Decoding Kentucky’s Medicaid Fee Schedule: What Beneficiaries Need to Know
Decoding Kentucky’s Medicaid Fee Schedule: What Beneficiaries Need to Know
Kentucky’s Medicaid Fee Schedule is a critical gateway to accessing affordable healthcare, translating federal mandates into state-specific reimbursement rates for providers and determining cost-sharing obligations for enrollees. From pharmacists to primary care physicians, understanding how fees are structured and applied can mean the difference between accessible care and unexpected out-of-pocket costs. As the state’s Medicaid program continues to expand under recent policy reforms, the fee schedule remains a dynamic, complex framework balancing cost containment with quality access.
This article unpacks the key components, coverage details, and real-world impact of Kentucky’s Medicaid fee schedule, offering essential guidance for patients and providers alike.
The Blueprint of Access: How Kentucky’s Medicaid Fee Schedule Works
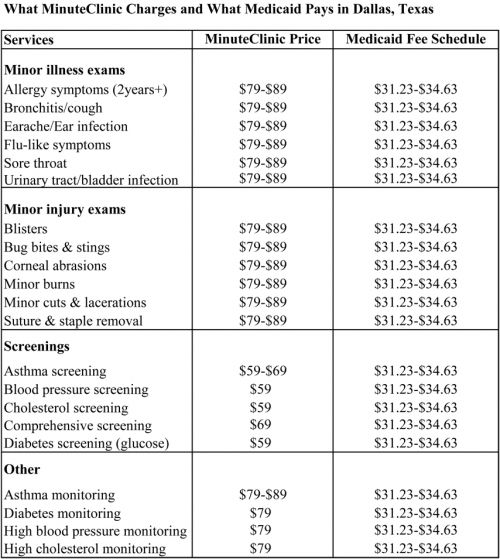
At its core, Kentucky’s Medicaid Fee Schedule serves as a standardized pricing mechanism governing what healthcare services are covered and at what cost to beneficiaries. Administered by the Kentucky Health Insurance Program (KHIP), the schedule reflects negotiated reimbursement rates between the state and healthcare providers—hospitals, clinics, pharmacies, and physicians—approved under federal Medicaid guidelines. These rates dictate both in-network payments and patient cost-sharing, including deductibles, coinsurance, and copayments.
The schedule is divided into multiple categories, primarily categorizing services by type and necessity. Categories such as “Renal Replacement Therapy,” “Psychiatric Evaluation,” and “Prescription Medications” have tiered fee schedules reflecting clinical complexity and cost variation. For instance, specialty pharmaceuticals may carry significantly higher reimbursement rates due to manufacturing costs and clinical monitoring requirements, while routine primary care services are priced according to national benchmarks with state-specific adjustments.
Providers must maintain current certification under the federallyhosted Medicaid (“Medicaid Rate Certification”) program, ensuring their service codes align precisely with scheduled fees. Failure to comply risks claim denials and delayed reimbursements, directly affecting clinic stability and ultimately, patient access.
Structure and Coding: Understanding Service Categories and Fee Determination
Kentucky’s fee schedule organizes healthcare services into detailed coding hierarchies, often using the Current Procedural Terminology (CPT) system to identify specific codes, which are then mapped to corresponding monetary values. These codes help ensure consistency and transparency in billing across the state’s Medicaid provider network.
Broad service categories include: - Primary Care Office Visits - Inpatient and Outpatient Hospital Stays - Laboratory and Diagnostic Services - Prescription Drugs - Mental Health and Substance Use Disorder Treatment - Transportation and Durable Medical Equipment Each category may include multiple subcodes representing service variations—such as scheduled vs. dose-reduced medications or virtual visits versus in-person consultations—directly affecting reimbursement scales. This granular categorization allows Kentucky’s Medicaid program to adjust pricing dynamically, recognizing differing levels of provider effort and resource use while keeping costs predictable and equitable.
Prescription Medications: A Key Component Under the Fee Schedule
Pharmaceutical coverage under the Kentucky Medicaid Fee Schedule is both a major cost driver and a vital component of care continuity.
The state maintains a scheduled formulary tied closely to the fee schedule, specifying reimbursement rates for both brand-name and generic medications. These rates are periodically updated based on pharmaceutical pricing trends, therapeutic equivalency, and clinical evidence. For beneficiaries, this means medications must fall within an identifiable tier to trigger the applicable fee—copays or coinsurance rates vary significantly by category.
For example: - Generic antibiotics may carry low copays (as low as $2–$10 per fill), - Specialty biologics used in treating autoimmune diseases can range from $300 to over $1,000 per claim, - Insulin and essential devices, critical for diabetes and mobility, are capped at minimal patient costs. Kentucky’s transparent formulary system helps reduce surprise billing, yet benefitees are advised to review their coverage annually, as tier placements and reimbursement tiers may shift. Pharmacists play a crucial role here, cross-checking prescription codes against the fee schedule to confirm coverage and advise on lowest-cost alternatives.
Out-of-Pocket Costs: How the Fee Schedule Shapes Beneficiary Expenses
The fee schedule directly influences how much Kentucky Medicaid enrollees pay at the point of service.
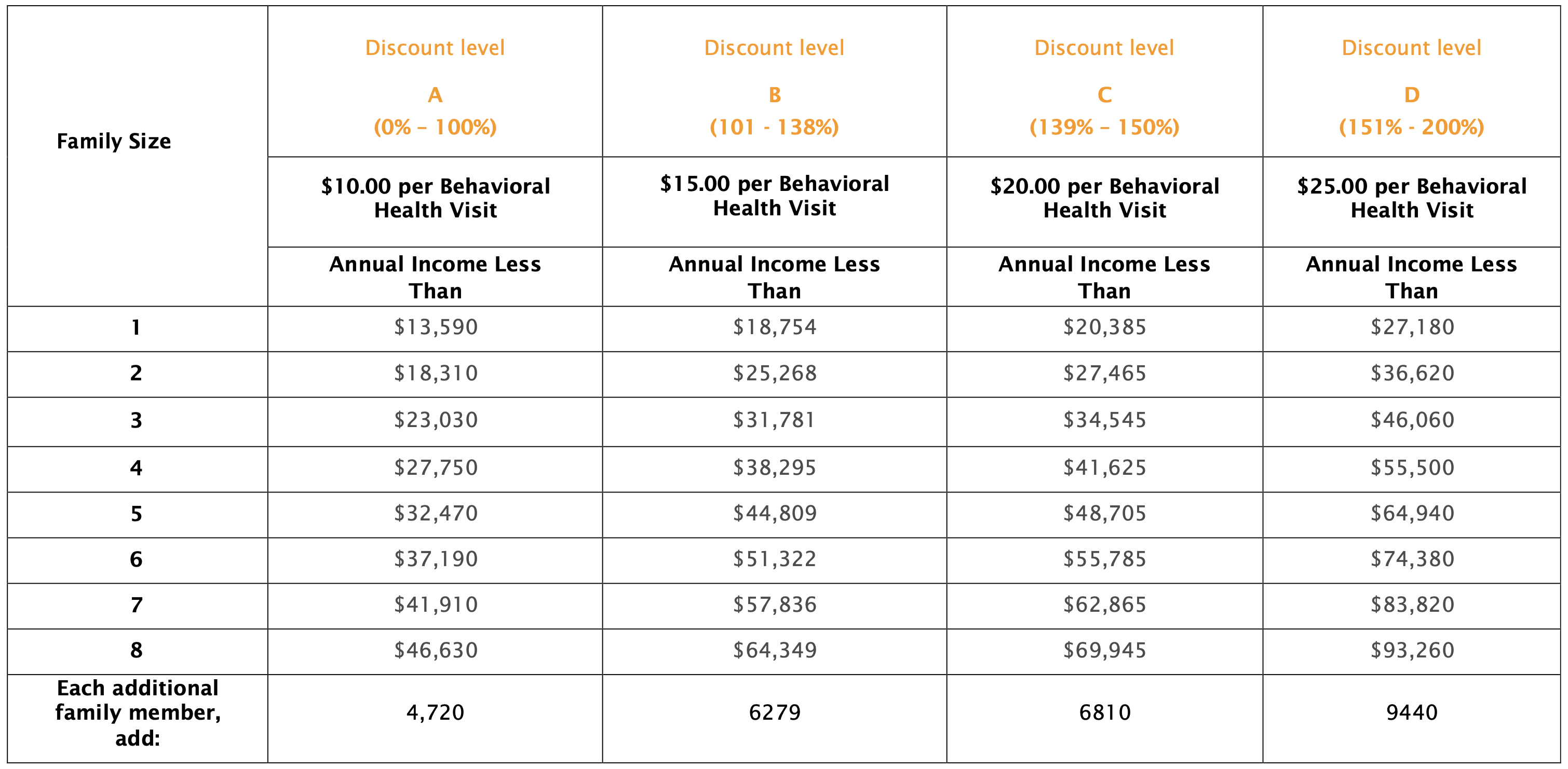
Cost-sharing includes deductibles, coinsurance, copayments, and sometimes Medicaid-specific surcharges. Understanding these elements is essential to budgeting for care. Common cost-sharing structures include: - Fixed copays for primary care visits ($15–$30), - Percentage-based coinsurance for specialist visits ($20–$50 depending on income) - Tiered prescription copays, as outlined above - Deductibles that must be met before full coverage begins, typically $200–$500 annually for individual enrollees These figures represent real-world expenses; low-income beneficiaries may qualify for full fee waivers, ensuring essential services remain accessible regardless of financial status.
The schedule also adjusts for categories deemed high-value for health outcomes, such as maternal care or chronic disease management, where copays may be waived or reduced to encourage timely care.
Moreover, the schedule integrates cost-containment measures like prior authorization for high-cost services and tiered prior authorization thresholds, reducing unnecessary care without blocking critical access. This balance ensures long-term fiscal sustainability while protecting beneficiary well-being.
Real-World Impact: Case Example of Fee Schedule in Action
Consider a low-income Kentuckian managing type 2 diabetes.
Each month, their regimen includes insulin ($80 copay), A1C monitoring visits ($40 copay), and prescription not refills ($25 copay). Under the 2024 fee schedule: - Insulin is fully covered after a $400 annual deductible, ensuring economic access. - Doctor visits carry $30 coinsurance,5 ensuring continuity.
- Generic diabetic medications are 100% covered post-deductible, minimizing ongoing burden. Compare this to an uninsured adult with the same condition: out-of-pocket costs could exceed $300 monthly, significantly deterring care adherence. This illustrates how the fee schedule directly reduces financial barriers, particularly for vulnerable populations, aligning policy goals with clinical necessity.
Regulatory Oversight and Ongoing Reform
Kentucky’s Medicaid Fee Schedule is not static; it evolves in response to clinical advancements, economic shifts, and policy priorities.
The state’s Office of Medicaid Program Management (OMPM) regularly reviews and updates schedule rates, often in consultation with the Kentucky Medical Association, pharmacy groups, and patient advocates. Federal CMS guidelines further constrain adjustments, requiring alignment with benchmarks for relative value units (RVUs) and regional cost indices. Recent reforms, including the expansion of telehealth reimbursement and specialty pharmacy carve-outs, reflect efforts to modernize coverage.
These updates aim to enhance access to emerging therapies while maintaining fiscal discipline. Transparency is increasingly emphasized, with public dashboards now available showing facility participation, fee tiers, and average reimbursement amounts—empowering beneficiaries to make informed decisions.
Looking Ahead: The Future of Kentucky’s Medicaid Pricing Landscape
As healthcare costs rise nationally, Kentucky’s Medicaid Fee Schedule faces mounting pressure to remain both affordable and equitable. Emerging trends—such as value-based payment models“ shifting reimbursement from volume to outcomes“ and expanded integration of home-based care—are poised to reshape fee structures.
Predictive analytics and real-time data monitoring will likely refine fee setting, enabling more precise alignment between service value and cost. Stakeholders agree that continued stakeholder engagement—patients, providers, and financiers—is critical. By grounding policy in evidence, equity, and adaptability, Kentucky’s Medicaid fee schedule will remain a cornerstone of accessible, sustainable healthcare for millions.

Related Post

Unlocking Kentucky’s 2024 Medicaid Fee Schedule: What Providers and Residents Need to Know

Unlocking the Green Flag Emoji: Decoding Its Hidden Meaning, Powerful Usage, and Surprising Popularity

Is Sara Saffari Dating Anyone? Unveiling the Truth Behind the Celebrity’s Romantic Life

Asstr Org Father Daughter: Navigating Love, Legacy, and Identity Across Generations

