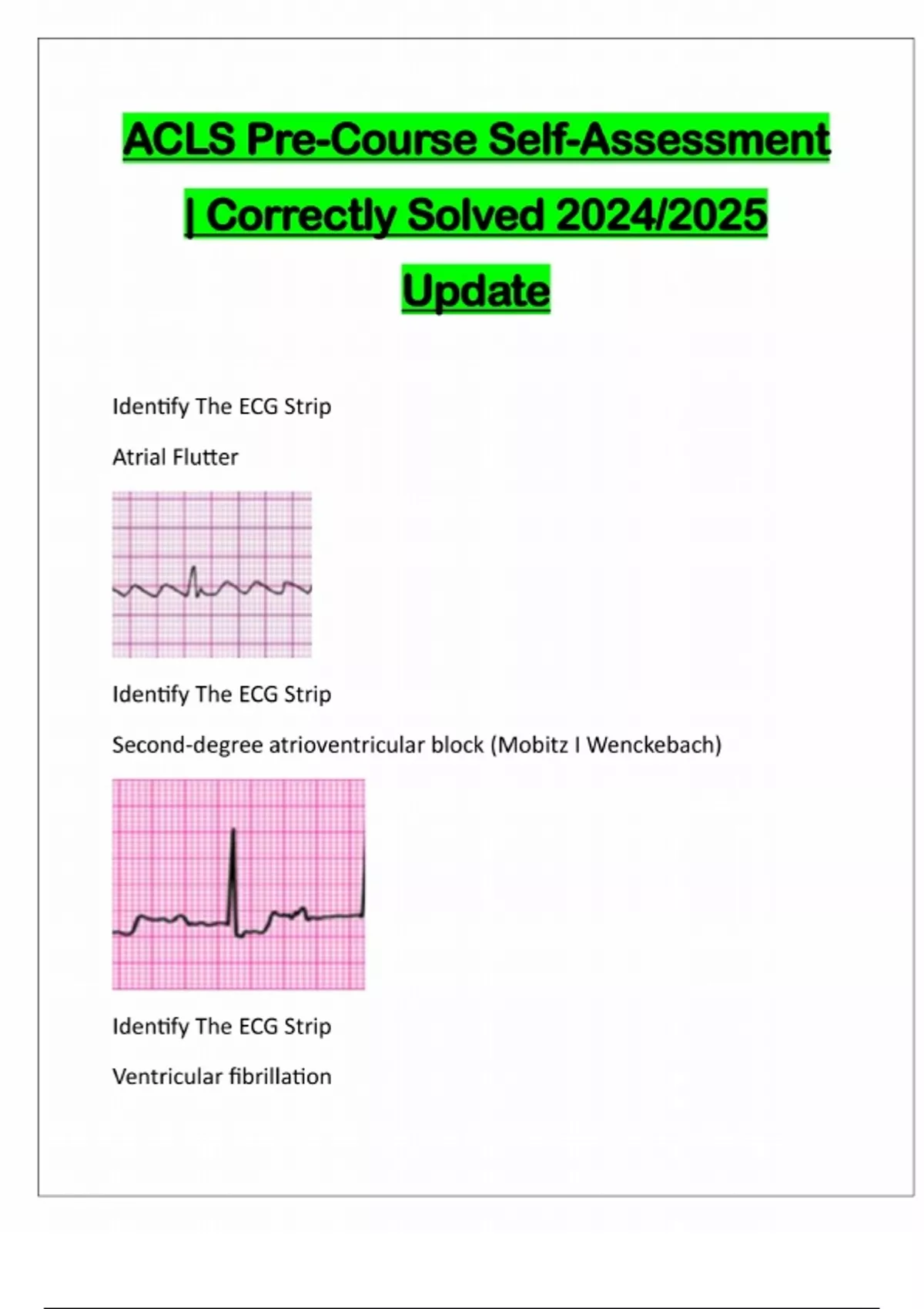
Acls Precourse Self Assessment: The Critical First Line in Emergency Triage
Acls Precourse Self Assessment: The Critical First Line in Emergency Triage
Emergency medical responders face split-second decisions where clarity and precision can mean the difference between life and death. The Acls Precourse Self Assessment stands at the forefront of this high-stakes environment, offering healthcare professionals a structured, early evaluation tool to rapidly assess patients before full Advanced Cardiac Life Support protocols activate. This foundational assessment guides clinical judgment, streamlines treatment pathways, and embeds pattern recognition in time-critical care—making it indispensable in modern emergency medicine.
The Essential Role of Precursory Assessment in ACLs
Rooted in the broader Acls framework—Advanced Cardiac Life Support’s precision-oriented approach—the Precourse Self Assessment serves as an initial triage benchmark.
Unlike full-scale ACLs, which demand comprehensive systemic evaluation including airway, breathing, circulation, and disability, the Precourse allows rapid initial data gathering. This early stage enables responders to categorize patients by severity, identify urgent threats, and prioritize interventions that prevent deterioration. As one emergency physician notes, “It’s not about doing everything—it’s about knowing what to do first.”
The assessment integrates vital signs, witness history, and basic physical exam findings to form a clinical snapshot.
Key indicators include pulse rate, mental status, respiration patterns, and signs of shock or circulatory compromise. “Timeliness matters—every second counts,” explains Dr. Elena Torres, a critical care specialist, “and the Precourse self check soothes the chaos by focusing intent.” By distilling complex presentations into actionable data, this tool empowers even less experienced clinicians to make confident, evidence-based choices.
Core Components of the Precourse Self Assessment Tool
The assessment is neither exhaustive nor haphazard; it follows a targeted protocol designed for speed without sacrificing diagnostic rigor.
It focuses on defining key physiological domains critical to hemodynamic stability and neurological integrity. - **Vital Sign Analysis**: Examining heart rate, blood pressure, respiratory rate, oxygen saturation, and temperature provides immediate insights into cardiac output, ventilation adequacy, and perfusion status. - **Mental Status Evaluation**: A simple Gross Motor Rating or the AVPU scale (Alert, Voice, Pain, Unresponsive) reveals neurological function, helping detect early cerebral hypoperfusion.
- **Airway and Breathing Assessment**: Checking for airway patency, airway obstruction signs, and effective respiration rates guides decisions on supplemental oxygen, airway adjuncts, or Bedford interventions. - **Circulation Insight**: Evaluating pulse quality, capillary refill, and peripheral perfusion flags ongoing shock or hemorrhage. - **Initial Pain and Trauma Screening**: Identifying pain level and visible injuries shapes pain management and trauma prioritization.
This integrated model reflects the Acls philosophy that structured assessment precedes effective intervention. By emphasizing concise, real-time evaluation, the Precourse tool avoids common pitfalls like delayed recognition of silent deterioration or misinterpretation of ambiguous symptoms.
Why Speed and Simplicity Matter in High-Stakes Scenarios
In cardiac arrest, SCA, or massive trauma, the window between symptom onset and collapse is often measured in minutes. The Precourse Self Assessment thrives on its ability to compress complex clinical analysis into structured, repeatable steps.
“It’s the difference between localizing a guided drill in a crisis and spinning aimlessly,” says paramedic and Acls instructor James Chen. “Familiarity with the tool builds muscle memory—improving response time by up to 30%.”
The simplicity of the tool ensures consistent application across varied settings—from ambulances and emergency departments to pre-hospital scenes and community first-aid sites. Training programs incorporating the Precourse report higher retention of ACLs protocols, as learners internalize key focus areas through repetition.
Moreover, by standardizing initial data collection, team coordination improves: nurses and EMTs communicate concerns with clarity, reducing ambiguity during handoffs.
Real-World Application: From Theory to救命行动
Consider a 58-year-old male collapsing in a public setting. On scene, a paramedic performs a Precourse Self Assessment: blood pressure 80/50 mmHg, RR 28, AWPNOU (Ab嬳cious-Verbal, Au-comfortable, No-verbal, Unresponsive), SpO2 91% on room air, pulse 110. Within 15 seconds, this triggers immediate action—begin high-flow oxygen, initiate IV access, prep epinephrine—all while awaiting advanced team arrival.
“We’re not waiting for a full exam,” notes a crisis team coordinator, “we’re using the key signs to drive urgency and precision.”
In hospital EDs, nurses employ the Precourse model during rapid response evaluations to quickly flag deteriorating patients. For example, a subtle drop in systolic blood pressure or altered mental status identified through the tool can prompt early resuscitation, preventing full-blown cardiac arrest. This early intervention cascade saves lives—studies show that recognition within the first 5 minutes of symptom onset improves survival by 20–40% in myocardial infarction and trauma.
Integration with ACLs Protocol: A Seamless Clinical Bridge
The Precourse Self Assessment does not operate in isolation; it seamlessly feeds into the full Advanced Cardiac Life Support algorithm.
Once the initial evaluation identifies an urgent threat—such as a collapsed Herz, dysrhythmia, or airway compromise—the tool triggers activation of ACLs protocols, including advanced airway management, defibrillation, and vasopressor use. This continuity ensures that the initial snapshot directly informs escalating interventions without cognitive dissonance.
For example, if the Precourse identifies bradycardia with hypotension, the protocol immediately shifts to sigmoid pacemaker check and atropine administration. Similarly, altered mental status points to hypoxic, hypovolemic, or toxic etiologies requiring immediate oxygenation and neurological diagnostics.
“It creates a narrative—each node builds on the last,” explains Dr. Marta Lopez, emergency medicine director. “The Precourse is not just a screen; it’s the first chapter in a dynamic clinical story.”
Educational and Training Implications
Incorporating the Precourse Self Assessment into first responder and clinician training transforms passive learning into active skill development.
Simulated scenarios using this tool reinforce pattern recognition, decision-making under pressure, and accurate documentation—core competencies for Acls certification. Training modules often combine classroom instruction with distributed practice, where repeated exposure to real-time assessments strengthens neural pathways. Research confirms that systematic muscle memory training reduces diagnostic errors by up to 50% in chaotic environments.
Standardization is critical. When teams train on the same criteria—using consistent terminology, scoring methods, and prioritization logic—they achieve greater coordination and trust. This uniformity directly translates to improved outcomes during actual emergencies.
Future Directions: Digital Integration and AI Support
Emerging technologies are enhancing the Precourse Self Assessment’s reach and accuracy. Mobile apps now offer guided assessments with real-time scoring, reducing variability among users.
AI algorithms, trained on thousands of clinical cases, support decision support by flagging subtle warning signs that might be missed in high-stress moments. Wearable biosensors coupled with prehospital alert systems could automate initial vital sign capture, feeding data directly into assessment tools. “The goal is not automation replacing clinicians,” cautions Dr.
Chen, “but augmentation—giving frontline providers faster, more precise foundations to act upon.” Such innovations promise to expand access to high-quality triage, particularly in rural or resource-limited settings.
The Acls Precourse Self Assessment endures as a vital bridge between instinct and expertise. Its structured simplicity, rapid deployment, and integration within ACLs protocols make it indispensable in the high-stakes world of emergency medicine. By focusing attention on the most consequential early indicators, it empowers responders to see clearly amid chaos—and act decisively before time runs out.


Related Post

Sabreena Brar: Redefining Social Media Influence in the Digital Age

John Mallory Asher: A Deep Dive Into His Life And Career
<strong>The Iron Ingot Skyrim Id: Forging Legend in Divine Steel</strong>

Top 10 Slow Jazz Instrumentals That Drift Like Mist — Perfect for Deep Relaxation

